Osteoporosis is a common condition where bones become weak that affects both men and women, mainly as they grow older. Bone is living tissue that is in a constant state of regeneration. That is, the body removes old bone (called bone resorption) and replaces it with new bone (bone formation). By their mid30s, most people begin to slowly lose more bone than can be replaced. As a result, bones become thinner and weaker in structure.
Osteoporosis is silent because there are no symptoms (what you feel). It may come to your attention only after you break a bone. When you have this condition, a fracture can occur even after a minor injury, such as a fall. The most common fractures occur at the spine, wrist and hip. Spine and hip fractures, in particular, may lead to chronic (longterm) pain and disability, and even death. The main goal of treating osteoporosis is to prevent such fractures in the first place.
Fortunately, you can take steps to reduce your risk of osteoporosis. By doing so, you can avoid the often disabling broken bones (fractures) that can result from this condition. If you already have osteoporosis, new medications are available to slow or even stop the bones from getting weaker. These medicines also can decrease the chance of having a fracture.
Fast Facts
Osteoporosis results from a loss of bone mass (measured as bone density) and from a change in bone structure. Many factors will raise your risk of developing osteoporosis and breaking a bone. You can change some of these risk factors, but not others. Recognizing your risk factors is important so you can take steps to prevent this condition or treat it before it becomes worse.
![]()
Age is not the only risk factor for osteoporosis. Lifestyle choices, certain diseases and even medications can lead to this condition.
![]()
A simple test known as a bone density scan can give important information about your bone health. Newer medications can slow and even stop the progression of bones getting weaker, and can help decrease fracture risk.
![]()
![]()
What causes osteoporosis?
Osteoporosis results from a loss of bone mass (measured as bone density) and from a change in bone structure. Many factors will raise your risk of developing osteoporosis and breaking a bone. You can change some of these risk factors, but not others. Recognizing your risk factors is important so you can take steps to prevent this condition or treat it before it becomes worse.
Major risk factors that you cannot change include:
Older age (starting in the mid30s but more likely with advancing age)
![]()
NonHispanic white or Asian ethnic background
![]()
Small bone structure
![]()
Family history of osteoporosis or an osteoporosisrelated fracture in a parent or sibling Prior fracture due to a lowlevel injury, particularly after age 50
Risk factors that you may be able to change include:
Low levels of sex hormone, mainly estrogen in women (e.g., menopause)
![]()
The eating disorders anorexia nervosa and bulimia
![]()
Cigarette smoking
![]()
Alcohol abuse
![]()
Low calcium and vitamin D, from low intake in your diet or inadequate absorption in your gut
![]()
Sedentary (inactive) lifestyle or immobility
![]()
Certain medications, including the following:
![]()
glucocorticoid medications (also called corticosteroids), such as prednisone (brand names: Deltasone, Orasone, etc.) or prednisolone (Prelone); see fact sheet on glucocorticoidinduced osteoporosis (/IAm A/PatientCaregiver/DiseasesConditions/GlucocorticoidinducedOsteoperosis)
excess thyroid hormone replacement in those taking medications for low thyroid or hypothyroidism
heparin, a commonlyused blood thinner
![]()
some treatments that deplete sex hormones, such as anastrozole (Arimidex) and letrozole (Femara) to treat breast cancer or leuprorelin (Lupron) to treat prostate cancer and other health problems
![]()
Diseases that can affect bones
![]()
endocrine (hormone) diseases (hyperthyroidism, hyperparathyroidism, Cushing’s disease, etc.) inflammatory arthritis (rheumatoid arthritis (/IAmA/PatientCaregiver/DiseasesConditions/Rheumatoid Arthritis), ankylosing spondylitis (/IAmA/PatientCaregiver/DiseasesConditions/Spondyloarthritis), etc.)
![]()
![]()
Who gets osteoporosis?
Osteoporosis is more common in older women, mainly nonHispanic white and Asian women. Yet it can occur at any age, in men as well as women, and in all ethnic groups. People over age 50 are at greatest risk of developing osteoporosis and having related fractures. Over age 50, one in two women and one in six men will suffer an osteoporosisrelated fracture at some point in their lives. In the U.S., about 4.5 million women and 0.8 million men over the age of 50 have osteoporosis, according to 2005–06 data. These figures are lower than older estimates, suggesting that osteoporosis is decreasing in the population. This is consistent with recent trends seen in decreasing rates of hip fracture.
However, another 22.7 million women and 11.8 million men over age 50 have low bone mass (known as osteopenia). People with low bone mass are also at higher risk of fractures, but it is not as high as for people with osteoporosis. If bone loss continues, people with osteopenia can become osteoporotic.
How is osteoporosis diagnosed?
You can learn if you have osteoporosis by having a simple test that measures bone mineral density— sometimes called BMD. BMD —the amount of bone you have in a given area—is measured at different parts of your body. Often the measurements are at your spine and your hip, including a part of the hip called the femoral neck, at the top of the thighbone (femur). Dual energy Xray absorptiometry (referred to as DXA or DEXA and pronounced “dexuh”) is the best current test to measure BMD.
The test is quick and painless. It is similar to an Xray, but uses much less radiation. Even so, pregnant women should not have this test, to avoid any risk of harming the fetus. DXA test results are scored compared with the BMD of young, healthy people. This results in a measure called a Tscore. The scoring is as follows:
DXA Tscore Bone mineral density (BMD)
Not lower than –1.0 Normal
Between –1.0 and –2.5 Osteopenia (mild BMD loss)
2.5 or lower Osteoporosis
The risk of fracture most often is lower in people with osteopenia than those with osteoporosis. But, if bone loss continues, the risk of fracture increases.
How is osteoporosis treated?
If you have osteoporosis, your health care provider will advise the following:
Calcium. Make sure you are getting enough calcium in your diet or you might need to consider taking supplements. The National Osteoporosis Foundation recommends 1,000 milligrams (shortened as mg) per day for most adults and 1,200 mg per day for women over age 50 or men over age 70.
![]()
Vitamin D. Get adequate amounts of vitamin D, which is important to help your body absorb calcium from foods you eat. The recommended daily dose is 400–800 International Units (called IU) for adults younger than age 50, and 800–1,000 IU for those age 50 and older. (These are the current guidelines from the National Osteoporosis Foundation.) You may need a different dose depending on your blood level of vitamin D.
![]()
Physical activity. Get exercise most days, especially weightbearing exercise, such as walking.
![]()
Some people also will need medication. A number of medications are available for the prevention and/or treatment (“management”) of osteoporosis.
Bisphosphonates. The US Food and Drug Administration (better known as the FDA) has approved certain drugs called bisphosphonates to prevent and treat osteoporosis. This class of drugs (often called “anti resorptive” drugs) helps slow bone loss, and studies show they can decrease the risk of fractures. The Table shows the drug names and dosing (how often you receive the drug) of bisphosphonates approved in the US for management of osteoporosis.
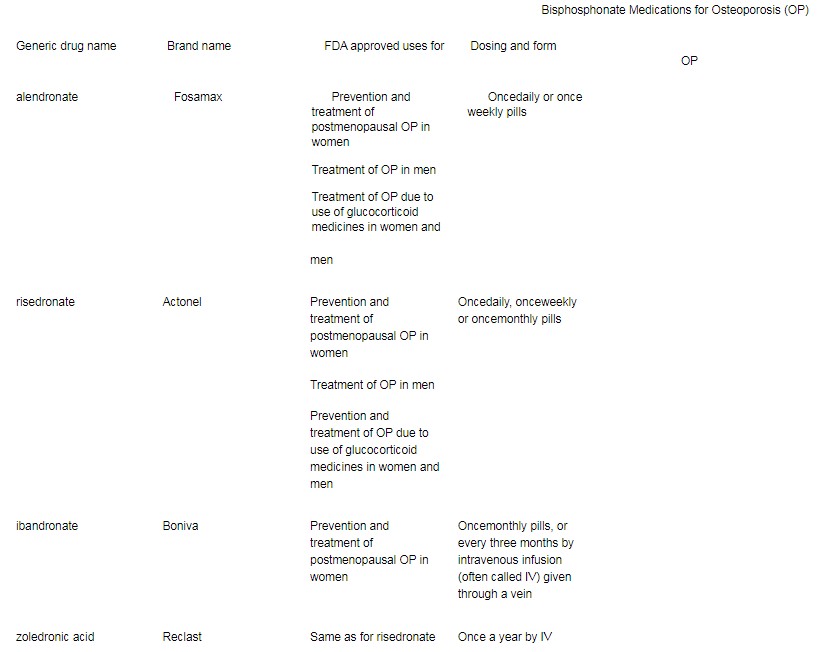
With all of these medications, you should make sure you are taking enough calcium and vitamin D, and that the vitamin D levels in your body are not low. (Your doctor can measure your vitamin D level with a blood test.) Alendronate, risedronate and ibandronate are pills that you must take on an empty stomach with water only, or else you will not properly absorb the medicine. These drugs sometimes can irritate the esophagus (the tube that goes from the throat to the stomach). Therefore, you should remain upright for at least an hour after taking these medications.
Other bisphosphonates include clodronate (Bonefos), etidronate (Didronel), pamidronate (Aredia) and tiludronate (Skelid). They are used to treat other bone diseases but are not FDA approved for osteoporosis treatment. In some other countries, clodronate is approved for osteoporosis treatment. The bisphosphonates are also used to treat cancer that has spread to the bones. The dose used is most often higher than for osteoporosis. Zoledronic acid used in cancer treatment is marketed under another name (Zometa).
There have been reports of rare side effects that may be linked to use of bisphosphonates. These include osteonecrosis of the jaw (/IAmA/PatientCaregiver/DiseasesConditions/OsteonecrosisoftheJawONJ) (also called jaw osteonecrosis or ONJ) and atypical femoral fractures:
Osteonecrosis of the jaw. There have been reports of ONJ (permanent damage of the bones of the jaw) resulting after use of bisphosphonates, mostly in people who recently had a dental procedure or had dental disease. Most cases were in people who received highdose IV bisphosphonates for cancer treatment. The risk of this problem in people taking these medications at doses recommended for osteoporosis management seems to be very low. Still, doctors recommend that anyone taking a bisphosphonate have good oral hygiene and regular dental care.
![]()
Atypical femoral fractures. Uncommon types of thighbone fractures have occurred in a small percent of people using bisphosphonates long term for their osteoporosis. Again, this risk appears to be very low, especially compared with the number of fractures that bisphosphonates prevent.
![]()
Calcitonin (Calcimar, Miacalcin). This medication, a hormone made from the thyroid gland, is given most often as a nasal spray or as an injection (shot) under the skin. It is FDA approved for the management of postmenopausal osteoporosis and helps prevent vertebral (spine) fractures. It also is helpful in controlling pain after an osteoporotic vertebral fracture.
Estrogen or hormone replacement therapy. Estrogen treatment alone or combined with another hormone, progestin, has been shown to decrease the risk of osteoporosis and osteoporotic fractures in women. However, combination estrogen and progestin can increase the risk of breast cancer, strokes, heart attacks and blood clots. Estrogens alone may raise the risk of strokes. Consult with your doctor about whether hormone replacement therapy is right for you.
Selective estrogen receptor modulators. These medications, often referred to as SERMs, mimic estrogen’s good effects on bones without some of the serious side effects such as breast cancer. However, there is still a risk of blood clots and stroke with use of SERMs. The SERM raloxifene (Evista) decreases the risk of spine fractures in women. It is approved for use only in postmenopausal women.
Teriparatide (Forteo). Teriparatide is a form of parathyroid hormone that helps stimulate bone formation. It is approved for use in postmenopausal women and men at high risk of osteoporotic fracture. It also is approved for treatment of glucocorticoidinduced osteoporosis. It is given as a daily injection under the skin and can be used for up to two years. If you have ever had radiation treatment or your parathyroid hormone levels are already too high, you may not be able to take this drug.
Strontium ranelate. This medicine is approved for managing postmenopausal osteoporosis in several countries around the world, but not the U.S. (Brand names include Protelos, Protos, Osseor, Bivalos, Protaxos and Ossum.) Studies show it lowers the fracture risk in postmenopausal women. The drug comes as a powder, which women dissolve in water and take daily. Because of an increased risk of blood clots, it should be used with caution in women who have a history of or risk of blood clots such as deep venous thrombosis or pulmonary embolism.
Denosumab (Prolia). This new class of “antiresorptive” drug is a fully human monoclonal antibody, a type of immune therapy. It works against a protein that interferes with the survival of boneresorbing cells. This treatment is approved for use in postmenopausal women who have osteoporosis and are at high risk of fracture. Another approved use is for women and men at high risk of bone loss and fractures from hormone depleting medications used to treat breast and prostate cancer. Patients receive this medicine as an injection under the skin every six months.
This medication can make your calcium levels go very low, so your calcium and vitamin D levels should not be low when you start to take this medicine. There may be an increased risk of infections when using this drug. There have also been rare reports of ONJ linked to use of denosumab. This drug is also approved for the treatment of cancer involving the bones, and is marketed under another name (XGEVA).
Pregnancy and osteoporosis
Young women who have risk factors for osteoporosis and fractures need to carefully consider their medication options if they are planning a pregnancy. None of the drugs for managing osteoporosis has enough safety data available to recommend using them in women who are pregnant or breastfeeding.
Bisphosphonates, even after you stop taking them, can stay in your body a long time. Animal studies show that bisphosphonates cross the mother’s placenta and enter the fetus. The risk of harm to the fetus in humans is not known. Thus, women who want to become pregnant later should weigh the expected benefits of bisphosphonates against the possible risks. If a woman who has taken a bisphosphonate becomes pregnant, she should have her blood calcium levels checked, because they could become low.
Preventing osteoporosis
Lifestyle changes may be the best way of preventing osteoporosis. Here are some tips:
Make sure you get enough calcium in your diet or through supplements (roughly 1,000–1,200 mg/day, but will depend on your age).
![]()
Get enough vitamin D (400–1,000 IU/day, depending on your age and your blood level of vitamin D
![]()
measured by your doctor).
Stop smoking.
![]()
Avoid excess alcohol intake: no more than two or three drinks a day.
![]()
Be physically active and do weightbearing exercises, like walking, most days each week. Aim for at least 2½ hours a week (30 minutes a day five times a week or 50 minutes a day three times a week), or as much as you can. Exercises that can improve balance, such as Tai Chi or yoga, may help prevent falls. Change lifestyle choices that raise your risk of osteoporosis. Implement strategies to help decrease your risk of falling.
You also should get treatment of any underlying medical problem that can cause osteoporosis. If you are on a medication that can cause osteoporosis, ask your doctor if you can lower the dose or take another type of medicine. Never change the dose or stop taking any medicine without speaking to your doctor first.
If you have low bone density and a high risk of breaking a bone, your doctor may suggest medicine to prevent your bones from getting weaker. (See the section “How is glucocorticoidosteoporosis treated?”) Health care providers now have a tool for estimating the risk of a patient’s having an osteoporotic fracture in the next 10 years call the fracture risk assessment tool (FRAX (http://www.shef.ac.uk/FRAX)). It was developed by the World Health Organization, and the score can help guide treatment decisions.
Living with osteoporosis
As doctors who are experts in diagnosing and treating diseases of the joints, muscles and bones, rheumatologists can help find the cause of osteoporosis. They can provide and monitor the best treatments for this condition.
The most serious health consequence of osteoporosis is a fracture. Spine and hip fractures especially may lead to chronic pain, longterm disability and even death. The main goal of treating osteoporosis is to prevent fractures. If you have osteoporosis, it is important to help prevent not just further bone loss but also a fracture. Here are some ways to decrease your chance of falls:
Use a walking aid. If you are unsteady, use a cane or walker.
![]()
Remove hazards in the home. Remove throw rugs. Also, remove or secure loose wires or cables that may make you trip. Add nightlights in the hallways leading to the bathroom. Install grab bars in the bathroom and nonskid mats near sinks and the tub.
![]()
Get help carrying or lifting heavy items. If you are not careful, you could fall, or even suffer a spine fracture without falling.
![]()
Wear sturdy shoes with soles that grip. This is above all true in winter or when it rains.
![]()
For more information
The American College of Rheumatology has compiled this list to give you a starting point for your own additional research. The ACR does not endorse or maintain these Web sites, and is not responsible for any information or claims provided on them. It is always best to talk with your rheumatologist for more information and before making any decisions about your care.
National Osteoporosis Foundation
www.nof.org (http://www.nof.org/)
National Institutes of Health Osteoporosis and Related Bone Diseases National Resource Center www.osteo.org (http://www.osteo.org/)
Updated May 2015. Written by Shreyasee Amin, MD CM, MPH, and reviewed by the American College of Rheumatology Communications and Marketing Committee. This information is provided for general education only. Individuals should consult a qualified health care provider for professional medical advice, diagnosis and treatment of a medical or health condition.
©2015 American College of Rheumatology
© 2015 American College of Rheumatology. All rights reserved.